Clinical Effectiveness of Hypnotherapy
The British Psychological Society
Hypnotherapy has a substantial and growing evidence base. In 2001, the Professional Affairs Board of the British Psychological Society (BPS) commissioned a working party of expert psychologists to publish a report entitled 'The Nature of Hypnosis'.1
Its remit was 'to provide a considered statement about hypnosis and important issues concerning its application and practice in a range of contexts, notably for clinical purposes, forensic investigation, academic research, entertainment and training.' (page 1).
It culminated with a concise summary of the current scientific research on hypnosis and opens by stating:
'Hypnosis is a valid subject for scientific study and research and a proven therapeutic medium.'
1 Heap, M., Alden, P., Brown, R.J., Naish, P. Oakley, D.A., Wagstaff, G., Walker, L.G. (2001) The Nature of Hypnosis: A Report Prepared by a Working Party at the Request of The Professional Affairs Board of the British Psychological Society. Leicester: BPS.
The Australian Psychological Society
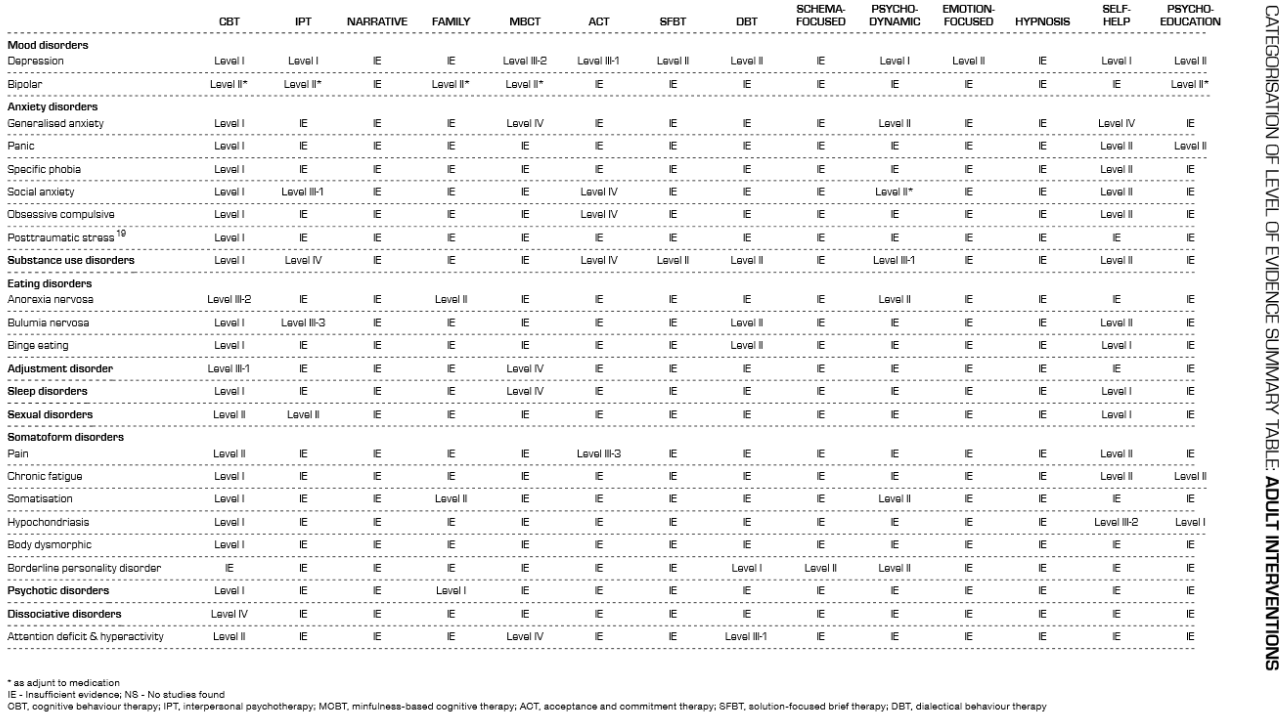
The literature review ‘Evidence-based Psychological Interventions in the Treatment of Mental Disorders’ Jan 2010: was unable to form conclusions on hypnotherapy due to insufficient evidence. As you will see from the extract below (p11), insufficient evidence (IE) afflicts many modalities.
There are, of course, many reasons for insufficient evidence. For example, some modalities – hypnotherapy included – receive relatively little research funding. So let’s look further afield…
National Institute for Health and Care Excellence and National Health Service (UK)
Hypnotherapy has been shown to be the most effective method for smoking cessation2 and is recommended by NICE/NHS as a treatment for irritable bowel syndrome:3
'Referral for psychological interventions
For people whose symptoms do not respond to pharmacological treatments after 12
months and who develop a continuing symptom profile (refractory IBS), consider referring
for:
– cognitive behavioural therapy (CBT)
– hypnotherapy
– psychological therapy.'
Since IBS is likely to be a psychosomatic illness, and hypnotherapists would tend to work with stress or implementation of dietary change, these other two uses for hypnotherapy are implicitly acknowledged by NICE.

Some theories at the interface between psychology and nutrition are considering the possibility that strong negative emotions, including stress, make the gut wall leaky to proteins that would normally be kept in the gut. Those proteins are then mistaken for pathogens and our immune system reacts with an inflammatory response. Hypnotherapy can deal with such emotions and memories.
2 Viswesvaran, C, & Schmidt, F.L. (1992) ‘A meta-analytic comparison of the effectiveness of smoking cessation methods‘. Journal of Applied Psychology. Vol. 77(4): 554-561
3 NICE IBS Quick Reference Guide, Feb 2008, page 4, and http://www.nice.org.uk/guidance/cg61/chapter/1-guidance

Chambless and Hollon
Hypnotherapy also meets the Chambless and Hollon criteria for empirically supported psychological therapies for a number of issues, including headaches, migraine, cancer pains, surgery pain and weight reduction.4
4 Chambless, D. L. & Hollon, S. D. (1998). ‘Defining empirically supported therapies.’ Journal of Consulting and Clinical Psychology. 66: 7-18
An example of research on efficacy
A study by Alladin and Alibhai5 investigated the effectiveness of cognitive hypnotherapy (CH) compared with cognitive-behavioral therapy (CBT) in the treatment of depression. 84 people with depression were randomly assigned to 16 weeks of treatment of either CH or CBT alone.
At the end of treatment, patients from both groups significantly improved compared to baseline scores. However, the CH group produced significantly larger changes in Beck Depression Inventory, Beck Anxiety Inventory, and Beck Hopelessness Scale. Effect size calculations showed that the CH group produced 6%, 5%, and 8% greater reduction in depression, anxiety, and hopelessness, respectively, over and above the CBT group.
The effect size was maintained at 6-month and 12-month follow-ups. The study represented the first controlled comparison of hypnotherapy with a well-established psychotherapy for depression, and met the APA criteria for a "probably efficacious" treatment for depression.
Further information
Research journals:
International Journal of Clinical and Experimental Hypnosis http://www.ijceh.com (includes an abstract search facility. It contains the abstracts from every single article published since the launch of the journal in 1953.)
American Journal of Clinical Hypnosis http://www.asch.net/ajch.htm
Robertson, D. (2008) 'Hypnotherapy as an empirically-supported treatment (EST)' The Hypnotherapy Journal. 1(9): 28-31
Books:
Nash, M.R. and Barnier, A.J. (2012) The Oxford Handbook of Hypnosis: Theory Research and Practice. Oxford: Oxford University Press
Heap, M. and Aravind, K (2001)
Hartland's Medical and Dental Hypnosis (4th ed.), London: Churchill Livingstone
Yapko, M. D., (2012) Trancework: An introduction to the practice of clinical hypnosis (4th ed.). NY: Routledge.
Databases and online resources:
The following databases routinely produce interesting results on searches for hypnotherapy research.
Academic
PsycInfo
Medline
ASSIA
Cochrane Library
Public
PubMed http://www.ncbi.nlm.nih.gov/pubmed
Search engines:
Google scholar: http://scholar.google.com.au and http://scholar.google.co.uk
Need more clarity on anything?
Feel free to contact us for a chat if you have any questions
Call to find out more

